Appropriate use of antibiotics for ear disease (2023)
Overview
We are delighted to announce that we have an esteemed guest, Dr Sue Paterson, who will be joining us to share her knowledge and expertise on the appropriate use of antibiotics in ear disease.
Dr Paterson is a renowned expert in the field, and her insights will be invaluable in helping us understand the most effective and appropriate use of antibiotics in the treatment of ear disease.
During the session, we will be exploring two key learning objectives:
Understanding the therapeutic options available when an infection is confirmed – including a discussion of the various types of antibiotics commonly prescribed and the factors to consider when selecting the most appropriate treatment.
How to establish if an infection is present – a critical step in determining the appropriate course of treatment and ensuring the patient receives the best possible care.
Presenters

Dr. Sue Paterson MA VetMB DVD DipECVD FRCVS
Dr Sue Paterson is an RCVS and European Board-Certified Veterinary Dermatologist. She is an elected Fellow of the RCVS in recognition of her contributions to clinical practice in the field of veterinary dermatology.
Sue has authored seven textbooks and published over 90 peer-reviewed articles in English, European, and American journals. She has lectured extensively across the globe, including at the NAVC Congress in the USA, the BSAVA Congress in the UK, and at multiple European Dermatology Congresses. She has also been a frequent speaker at the World Congress of Veterinary Dermatology (WCVD) and has delivered invited lectures in over 40 countries.
Sue is an elected member of RCVS Council, Chair of the Advancement of the Profession, and the Council lead for Sustainability and Leadership. She currently serves as President of the RCVS.
She is a past President of the BSAVA and the ESVD, and is the current President of the World Association for Veterinary Dermatology.
Sue is also a Trustee of Battersea Dogs and Cats Home. In her spare time, she enjoys long walks with her dogs across the Cumbrian fells, where she lives.
Transcript
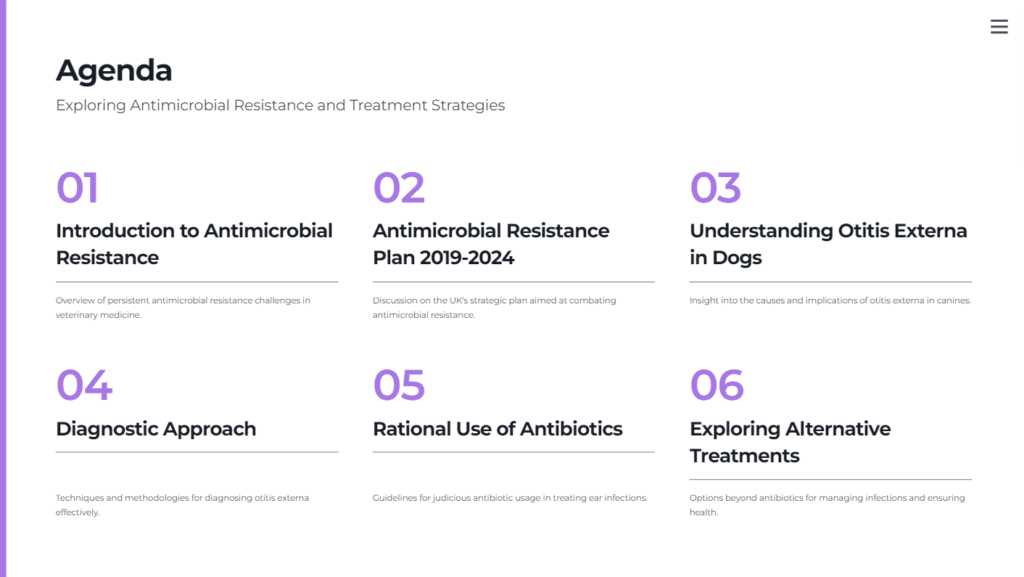
Hello and welcome to this presentation coinciding with Antimicrobial Awareness Week. I want to start by discussing the UK government’s Antimicrobial Resistance Plan, published in January 2019. This plan, which runs through 2024, outlines steps for medical and veterinary professionals to combat antimicrobial resistance.
The plan presents some concerning statistics: 123 countries report extensive multi-drug resistance, up to 2 billion people lack access to antimicrobials, and antibiotic consumption is expected to rise globally over the next decade. By 2030, 700,000 people could die from multi-resistant infections. Notably, no new classes of antibiotics have been discovered since the 1980s.
The plan sets out nine ambitions, three of which are particularly relevant for veterinary professionals: protecting animal health and welfare, demonstrating the appropriate use of antimicrobials, and engaging with the public about antimicrobial resistance. We need to discuss with clients whether antibiotics are truly necessary or if alternative treatments suffice.
It’s crucial not to simply reduce antibiotic usage, as this could compromise animal health. Instead, we should focus on using antibiotics when needed and seek alternatives, such as antiseptics, where possible. This is especially important in cases like otitis externa, which we’ll focus on today.
I’m Dr. Sue Patterson, a specialist in veterinary dermatology and director of Virtual Vet Derms. Today, we’ll discuss the rational use of antibiotics for treating otitis externa in dogs. Our learning objectives are to identify infections to determine antibiotic necessity, explore therapy options, and choose the appropriate antibiotics.
To decide if infection is present, we categorise otitis externa using the PPPS system: primary causes (underlying factors), predisposing factors (susceptibility enhancers), secondary causes (infections), and perpetuating factors (chronic changes). We aim to identify the primary cause, treat the infection, and restore normal ear anatomy to prevent recurrence.
Yeast and bacteria are secondary causes of infection, triggered by factors like allergies or environmental conditions. Cytology is essential to confirm infection, offering a clear picture of what’s happening in the ear. I recommend examining both stained and unstained samples to detect parasites and assess bacterial presence in chronic cases.
When taking ear samples, approach the animal gently to avoid stress. After assessing for pain, use a cotton swab to collect a sample from the ear canal, then roll it onto a slide. Stain the sample using a three-step process and examine it under a microscope for inflammatory cells and pathogens.
Cytology helps determine whether an infection involves yeast, bacteria, or both. It can also reveal if we’re dealing with cocci or rod bacteria, influencing treatment choices.
Regarding therapy, we focus on three steps: cleaning the ear, using steroids to reduce inflammation, and treating the infection. Ear cleaning is crucial, as discharge can block examination and treatment effectiveness. Cleaning provides pain relief and enhances the efficacy of antiseptics and antibiotics.
Steroids help reduce ear canal swelling, allowing better penetration of treatments. Prednisolone is often used for its anti-inflammatory effects. Systemic and topical steroids can reduce swelling and discharge, making treatments more effective.
For treating infections, clean the ear to remove wax and improve treatment absorption. There are various antiseptics effective against yeast in the ear. Our approach involves using antiseptics and antibiotics judiciously to manage infections while preserving the animal’s overall health and welfare.
When dealing with otitis externa, it’s essential to choose antibiotics that have a narrow spectrum of activity specifically targeting pathogens like Staphylococcus, which are frequently encountered in ear infections. Using antibiotics with broad spectrums, such as fluoroquinolones, should be avoided unless there is documented resistance to more targeted antibiotics and antiseptics.
In cases where rod bacteria, like Pseudomonas, are present, biofilms often form early. This requires the use of cleaning products with biofilm-busting activity. Effective options might include products containing TRIZ EDTA, N-acetylcysteine, or hypochlorous acid. These are useful for breaking up discharge and are active against gram-negative infections. Sometimes, starting with an antiseptic in combination with steroids to reduce swelling and discharge is preferable. However, if antibiotics are necessary, aminoglycosides such as gentamicin should be considered first. These are particularly effective against Pseudomonas infections, especially when the ear canal is clean.
The European Medicines Agency (EMA) has provided guidelines categorizing topical otic antibiotics into four groups based on their recommended usage:
- Group D (Use with prudence): This includes fusidic acid, which is very effective against gram-positive organisms like Staphylococcus and Streptococcus, but it has no activity against gram-negative bacteria or anaerobes. Fusidic acid should be considered in acute cases with cocci on cytology as a first-line treatment option.
- Group C (Use with caution): This group comprises aminoglycosides and florfenicol, which have a broader spectrum of activity. Aminoglycosides are effective against Staphylococcus, including methicillin-resistant strains, and have good activity against gram-negative bacteria such as Pseudomonas. Florfenicol is primarily effective against gram-positive bacteria and is an option for Staphylococcus infections alongside fusidic acid.
- Group B (Restrict): This group includes polymyxins and fluoroquinolones. These should be reserved for more difficult cases due to their significant effectiveness against gram-negative bacteria, including Pseudomonas aeruginosa. Polymyxin, although synergistic with myconazole against gram-positive bacteria, should mainly be used for challenging gram-negative infections.
- Group A (Inappropriate for use): This group contains drugs such as ticarcillin and carbenicillin, which are generally not recommended for use in dogs’ ears.
When selecting antibiotics, cytology plays a crucial role. Identifying cocci, rods, or yeast on cytology helps determine the most appropriate treatment. For instance, cocci might be treated with a narrow-spectrum drug or antiseptic, while rods indicate a need for biofilm-busting agents and drugs with strong gram-negative activity.
In acute Staphylococcus infections with minimal discharge and swelling, fusidic acid combined with a mild steroid like prednisolone is often sufficient. For more chronic cases with significant swelling and discharge, a stronger steroid such as mometasone or betamethasone might be needed, in combination with florfenicol.
Pseudomonas infections tend to be more severe, characterized by a swollen, ulcerated ear canal filled with greenish-yellow mucoid discharge. The canal often narrows and may show a hemorrhagic discharge as the condition becomes chronic. If the eardrum is intact, starting treatment with an aminoglycoside such as gentamicin is advised. If resistance develops or the infection becomes chronic, consider moving to more potent antibiotics like polymyxin or fluoroquinolones. The choice of product should consider both the antibiotic and steroid content, depending on the severity of the swelling and discharge.
It is crucial to combine clinical signs with cytology when assessing for infection, as relying solely on clinical signs can be misleading. Ear cleaning should be an integral part of the treatment protocol, as many antibiotics are ineffective if the ear is not clean. Steroids should be used both topically and systemically to manage inflammation and discharge. Antiseptics can serve as the first line of defence, reserving antibiotics for cases where they are truly needed and adhering to EMA guidelines to maintain antibiotic efficacy.
By following these principles and choosing antibiotics wisely, veterinary professionals can ensure they provide optimal care while preserving antibiotic availability for the future.




